The future is here, and it’s not what we thought it would be. But screw flying cars and hoverboards—where is our legit birth control?
I remember reading Brave New World for the first time and picturing Lenina and Fanny Crowne prancing around the exercise lawn after dosing themselves with soma and completing the Malthusian Drill. The book came out in 1931, a year after scientists isolated the hormones that would later be used in our primary forms of birth control, but it wasn’t until 30 years later that “the pill” became available—a decade longer if you were “unwed.”
Videos by VICE
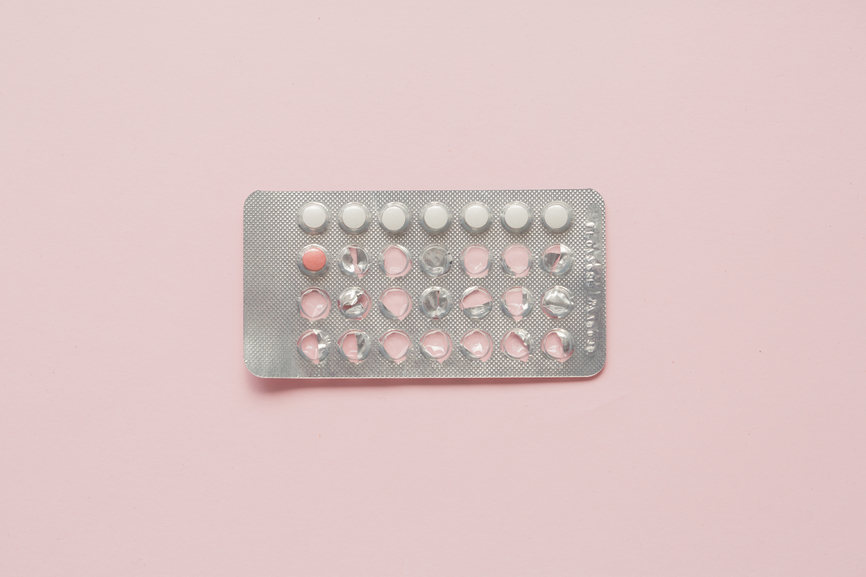
In present day 2015, the available options aren’t great, and the burden still rests largely on women to mitigate the damages of our wanton impulses. Aside from the copper IUD, all the birth control devices and pharmaceuticals available to women alter our hormones with various weird side effects. When it comes to birth control for men, aside from condoms and pulling out (neither of which are very reliable in practice), a vasectomy has been the only other option for preventing unwanted pregnancies. Though there’s about a coin-flip chance of it being reversible, those odds aren’t enough to make it something guys under 40 typically consider. A few other male contraceptives are being explored, but there are no approved male contraceptive drugs in the United States (which was confirmed to me by US Food and Drug Administration spokesperson Andrea Fischer).
But what if there was a simple way a man to fire blanks until he and his partner were ready to have a kid—without the snip snap?
Medically, there is a way. It’s been studied in animals and humans for more than 30 years with almost no documented complications. Known as “the male birth control injection,” an application called RISUG (Reversible Inhibition of Sperm Under Guidance) was invented in India in the 1970s by Sujoy Guha, a professor of biomedical engineering at the Indian Institute of Technology. It’s affordable, minimally invasive, and fully reversible—and it’s the most effective, non-permanent way of preventing pregnancy (from the sperm side) the world has ever seen, according to studies so far.
In 2010, the US-based Parsemus Foundation, a not-for-profit organization with the mission of “finding low-cost solutions neglected by the pharmaceutical industry,” purchased the patent for RISUG for $100,000. The organization is currently focusing on a slightly different birth control injection called Vasalgel which has a better chance of going to market in the US.
With the exception of certain fetish circles, most people would agree: sharp objects + genitals = scary
The process takes about 15 minutes. A doctor injects a tiny dot of a synthetic gel into the sperm-carrying tube just outside of each testicle. Once injected, the gel sets in the tube and acts like a filter, allowing fluid to pass through but not sperm.
“Like water might percolate through Jello,” said Elaine Lissner, director of the Parsemus Foundation.
Related: How One Company Aims to Help Men Grow Their Foreskins Back
This isn’t like a Depo-Provera shot you have to get once every few months either—once injected, the sperm-filtering gel would remain in place for 10 years. If the recipient decides he wants to take a shot at having kids at any point in between, all it takes is another injection of sodium bicarbonate (aka baking soda) to dissolve the liquid, and the sperm factory becomes operational again.
It may sound too good to be true, but clinical and animal trials in India have shown that the method works with near-perfect results and no serious side effects. And unlike the birth control pill and condoms, which have a real-life efficacy rate far lower than the ‘perfect use’ scenarios advertised on the packages, the birth control injection, like an IUD, comes with virtually no room for human error.
“There’s nothing for you as a person to screw up,” said Aaron Hamlin, executive director of the Male Contraceptive Initiative. “When you have a method that doesn’t require you to remember to do anything, like Vasalgel, you get the injection into the vas deferens and walk out the door. After all that’s done, when it’s time for you to have sex, everything you’ve had to do is already done.”
So what happens to the sperm? Guha has hypothesized that they explode or be shredded into nonfunctional parts by the time they get to the other side. Others have ventured that the sperm can’t pass through the gel at all and are absorbed back into the body like other proteins, or are otherwise deactivated by the acidity or electromagnetic charge of the gel.
“It’s hard to tell what exactly happens to the sperm, except that they don’t come out the other end,” said David Sokal, co-founder of the Male Contraception Initiative and a former clinician.
But ok, I get it; with the exception of certain fetish circles, most people would agree: Sharp objects + genitals = scary. But what’s worse: a few pokes in the balls for 15 minutes and pregnancy-free sex for a decade, or giving up full agency over your life and freedom to care for the surprise child you will be shackled to for the next 18 years?
“There are loads of benefits for being able to suppress pregnancy or time it the way that you like,” Hamlin said.
Other guys recoil at the mention of anything involving “male birth control” because, unsurprisingly, there are misconceptions floating around about what the new technique involves. This is not a vasectomy—it isn’t even considered surgery. The vas deferens can be exposed without the use of a scalpel, simply by poking the scrotum with special forceps and spreading the skin apart over each tube. The resulting hole is so small it doesn’t even require stitches.
“A lot of times, you’ll hear some mistaken descriptions about Vasalgel—that the injection goes in your penis, which it doesn’t. That perhaps rightfully scares men… but it’s coming from a mistaken description,” Sokal said.
But I did encounter a few reasons to be skeptical of RISUG and its successor Vasalgel in my research. For one, the phase III clinical trial data on RISUG data isn’t public, and preliminary results that have been published are from a decade ago and with a small sample size. When I contacted the organization in charge of conducting the trials in India, the Indian Council for Medical Research (ICMR), Deputy Director General Radheys Sharma said they could not release information on the success rates and reversals to a foreign media outlet without first getting government approval, and has not responded for further comment.
I was able to reach Guha, the inventor of RISUG, who said he has been working on RISUG in India in coordination with the ICMR, supplying the medical syringes and advising on clinical trials. “Since I have not been called to give any assistance regarding subjects I presume that the there are no problems from the technical and medical point of view,” he wrote in an email.
Another strange aspect of the story is that early phase III clinical trials in India were “aborted” in 2002 for reasons the Indian Ministry of Health attributed to an undisclosed side effect, but no evidence of the purported side effect was ever reported by the doctors conducting the clinical trials in New Delhi.
Motherboard Video: The fight over whale hunting in the Faroe Islands
There have been no reports, in animal or human trials, of it not working, however, except for one participant in an Indian clinical trial who reported that his wife became pregnant after he was injected. (This was attributed to improper injection, but it’s not outside of the realm of possibility that his wife became impregnated by someone else.)
I did find one paper that listed some components of the polymer compounds in RISUG and Vasalgel as having been previously classified as carcinogenic because of effects observed in freak chemical factory accidents, but the amounts those people were exposed to were way larger than what’s used in the injection.
“I don’t actually think it’s a patriarchal plot that’s stopping it at this point. I think it’s money. It takes a lot of money.”
Perhaps the best reason to be skeptical of RISUG and Vasalgel from a scientific standpoint rests on a cultural factor: guys generally don’t want to talk about their balls with doctors. Getting them to follow up one, five, 10 years after the procedure is hard, and has been preventing researchers from collecting adequate data to prove to regulatory bodies that it works.
But the clinical trials that have been completed and publicised in India over the past three decades have shown great success—enough to catch the interest of the Parsemus Foundation, which has been investing the bulk of its efforts into expanding research for a male birth control injection in the US. Still, the future existence of what could possibly be the most practical solution to birth control invented in the past 100 years hinges on getting past two main obstacles: the Food and Drug Administration and shortage of money.
“I don’t actually think it’s a patriarchal plot that’s stopping it at this point,” Lissner said. “I think it’s money. It takes a lot of money.”
Because the FDA doesn’t recognize results from clinical trials conducted overseas, all the experiments done in India must be replicated in the US with larger sample sizes and with stricter guidelines for trial duration. Animal trials run anywhere from $200,000 to $300,000 a pop and, should the FDA permit clinical trials to take place in humans, “the next steps are millions of dollars,” Lissner said.
Between $5 to $10 million, to be more precise. While this project seems ideal for a large humanitarian organization to back, the response has been lukewarm. Lissner said that representatives of the Bill and Melinda Gates Foundation, for example, “don’t see the point in the male version” because their primary focus in contraceptives is options for women in developing nations. ” The science of contraception for men is less advanced, as is the proof of concept for men using contraception in the poorest countries of the world,” said Kellie Sloan, director of family planning at the Foundation, in a statement to Motherboard.
Count big pharma out as well—unlike big-ticket products, Vasalgel doesn’t have the ability to make the money back since it’s a one-time procedure using materials that are relatively inexpensive to make and distribute. Lissner pointed out that if the average person hits puberty at 13, and doesn’t want to have a kid until they’re in their mid-30s, that’s more than 20 years worth of contraception from which pharmaceutical companies can profit.
“The big pharma companies like drugs that people will take for years and years, that they have to take every day,” Sokal said. By contrast, the makers of RISUG have bragged that it costs less than the syringe used to inject it; Vasalgel would cost less than your typical $800 IUD.
“[Pharmaceutical companies] have a target that if they can’t make $500 million a year on a new drug, it’s not worth their time and energy to invest in it,” Sokal said, citing his conversations with pharmaceutical reps. By that estimate, it would take 625,000 injections a year to be of interest to big pharma—which is about 125,000 more procedures than there are annual vasectomies in the US.
And even if some genius publicity campaign made the male birth control injection wildly popular, why would the major pharmaceutical companies, all holding stakes in different forms of hormonal birth control, want it to exist?
Sokal doesn’t see a conspiracy—more of a failure to break through. “I don’t know if [the big pharma companies] are trying to torpedo the Vasalgel research. They probably don’t believe it’s a threat,” he said. “The major mainline scientists are ignoring this. It hasn’t really made a big media splash. Until they see clinical data, they’ll probably see the business as underfunded, that this is a long shot.”
When RISUG was first invented, it was classified as “an injectable, non-occlusive chemical,” but when the Parsemus Foundation began working on Vasalgel in the US, they opted to categorize it as an “injectable, non-occlusive contraceptive device” considered a “plug” or “filter” so they would have a better chance of FDA approval.
The Parsemus Foundation decided to stop pursuing research on RISUG as its primary effort and pursue a variant, Vasalgel, instead.
The main problem with RISUG was a lack of chemical stability as required by FDA standards. Because the main ingredient in RISUG acidifies while sitting in a packaged syringe over time, what goes into the syringe is often slightly different than what’s in the syringe after a year or more. To work around this, the foundation simply used RISUG’s acidic byproduct as the starting point and called it Vasalgel.
“We had to make a more shelf-stable version,” Lissner said. “We didn’t think we could get it through the FDA if we couldn’t prove it was stable. So we figured, why not just try the acid form off the bat, and see whether it works?” Initial animal studies in rabbits suggest Vasalgel works just as well as RISUG, but more studies will be needed to prove it’s as effective—and as safe.
“We’re taking a big gamble because it was just a one-year study. So hopefully it will be as durable as RISUG,” she said.
Currently, Guha is continuing his work developing RISUG at the Indian Institute of Technology in Kharagpur, India, and also via the private company IcubedG Ideas, of which he is one of four directors. He’s optimistic about the prospect of RISUG reaching consumers soon, at least in India.
Vasalgel is now estimated to be on the market by 2020
“Technical and Medical problems have been resolved and there is adequate funding. So at present there are no problems,” Guha told LadyBits in an email. When it comes to why the phase III trials have lasted so long, he stressed the standards of safety in India and the importance of following up with trial participants 10 years after the initial injection. “India does not go for slip shod method of moving ahead without reported pre clinical and clinical study results open to international scrutiny just to gain limelight and commercial benefits [sic].”
“Slip shod” or otherwise, Parsemus is giving hope to thousands of people who want Vasalgel; currently there are 22,000 men on the waiting list for clinical trials, according to Lissner.
“We’re not in touch with Dr. Guha or clear with where he stands,” Lissner said. “I hope he’s making progress. Either way you get to a solution, the world wins.”
According to Lissner, the majority of inquiries about Vasalgel come from people in their 20s— men looking for more control over their reproductive future, and women having problems with the available methods. The most vocal group of all, she said, is “the young men on the dating market who are concerned about an ‘oops’ with a condom or the pill. “I think as far as what’s holding things back, it’s definitely the idea that men 20 years ago weren’t interested. And maybe men 20 years ago weren’t. But men today sure are,” she said.
In May, the Parsemus Foundation is slated to release data from a Vasalgel study conducted on baboons. It intends to run a crowdfunding campaign this summer, and hopes to begin clinical trials early 2016. Though a smattering of articles from September 2014 hyped a 2017 launch for consumer availability of Vasalgel, Hamlin said that realistically, it’ll be more like 2020.
If it ever reaches shelves at all.
“Nobody has pulled up the scale of money and the focus to finish it,” Lissner said. Even if Vasalgel trials are successful, it remains unclear who’s going to make the male birth control injection for the rest of the world outside of the US and India. If the drug does appear in the next five years, maybe the humanitarian foundations will be compelled to step up.
Personally, I look forward to a future where the majority of guys are card-carrying members of the injection club—a world where teen pregnancy wouldn’t be the large-scale life-ruiner it is today, and women wouldn’t be forced to pump themselves full of hormones or undergo dangerous surgical procedures to ensure their continued childlessness. With some interesting innovations on the condom front up ahead, sex would be better and more worry-free than ever. Until then, we’re stuck with the same roulette wheel of birth control methods, even though we’ve had an answer for more than 30 years.
This article is part of Bodies of the Future, a collaboration between Motherboard and LadyBits. Follow LadyBits on Twitter and Facebook.