Many people think about transition—especially medical transition—as a process of going from point A to point B. From one gender to another. From clockable to passing. I’m non-binary, though, and I can tell you that that’s not always how transition goes.
In 2014, I began taking a low dose of hormones to achieve subtle masculinizing effects, a process that I call microdosing testosterone (or “T”). I had to mostly find my own way as I worked with doctors to figure out that process—scouring the internet for information before my non-binary transition, I found no resources about medically transitioning as an AFAB non-binary person aside from a few scant Reddit threads and a (miraculous) blog by Micah, a non-binary person who’s been exploring microdosing since 2011. After writing an article about my experience with microdosing in 2019, I received hundreds of DMs from people who wondered, as I had, about the intricacies of microdosing T as a non-binary person assigned female at birth.
Videos by VICE
As they and I both knew: It’s hard to know where to look for information about transitioning—or any aspect of medical care—when you’re non-binary, except asking other non-binary people about it. Trans and non-binary people are underdiagnosed and undertreated in every medical sense, not just in terms of their gender-related care: Twenty-three percent report not seeing a doctor when they need to for fear of mistreatment and 50 percent report needing to teach their providers about their gender identity. Almost none of the research about AFAB people’s medical transitions accounts for non-binary approaches to transition like microdosing. That’s what we know about on paper: just about nothing. Many standardized guides for hormone replacement therapy now include the word “non-binary,” but many providers remain resistant to any understanding of mine as a real identity, let alone how to care for people like me.
Inspired by the people asking me questions—just like how I turned to Micah’s work to inform my transition—I’ve put together this guide to help answer some of the questions people have sent me about microdosing testosterone as I’ve experienced it, along with medical backup from reputable experts and trans-focused studies and publications. I’ve done a lot of research—speaking with exceptional healthcare providers; reading Paul B. Preciado’s Testo Junkie; exchanging late-night DMs with other non-binary people—but I’m not a medical professional. Guides are almost never comprehensive, so consider this my disclaimer: I am one non-binary person, with one particular body. Hormones—no matter the dosage—affect everyone differently, in part because everyone’s body metabolizes testosterone differently. Consider this guide just one tool in your microdosing arsenal to support any medical treatment you might be considering.
I know you have a lot of questions! Here are my best answers, as someone who’s made, and is still making, themselves.
First of all… what is microdosing testosterone?
Microdosing testosterone means taking small doses of T to achieve less-than-maximal masculinizing effects over a prolonged period of time—in my case, three years and counting so far. This understanding fits within a GAHT—gender-affirming hormone treatment—framework of care. Changes can include a stronger jaw and increased body and facial hair, among many potential others. Microdosing is also sometimes referred to as “low-dose” testosterone. We will talk more about exactly all of this, in as much detail as possible, as we go.

How much T does a person take when they’re microdosing, and how do they take it?
It depends. To answer that, it’s important to know the average dose for AFAB people who are taking higher doses of T to achieve maximal masculinizing effects. For the purposes of this section, I’ll use UCSF Transgender Care as my main point of reference. It’s one of the leading organizations in transgender medicine and regularly pioneers cutting-edge technologies and research. According to its guide, a standard dose of T taken by anyone looking to achieve maximal masculinizing effects is about somewhere between 50mg–100mg every week for injections, or 4.5g–10g every day for transdermal testosterone administered through gel. In the U.S., testosterone also comes in the form of patches or creams, which you can find more information about at the link above.
Microdosing is taking any amount of T below that standard dose. A more specific number is even harder to approximate because there’s very little information out there, but can range from 20mg–40mg every week for injections and 2.5g–4.5g for transdermal testosterone aka testogel (dosage widely varies, as there are different strengths available). Testogel and patches may be harder to microdose with because packets come in specified dosages [2.5g to 5.0g]. Some people use half-packets, but patches are a bit more complicated—the most common ones have reservoirs of T in the middle, and cutting those will cause the dosage to leak out.
The thing to remember is that microdosing is less about the dosage, and more about the way that your body metabolizes hormones, so there is no fixed, perfect dose! Having used both injections and testogel, I fluctuate between 20mg–30 mg or 1.5g–2g daily, and have been in that range for roughly three years, on and off. I recently switched from injections to testogel because I was experiencing a lot of moodiness because of hormone level spikes, and my doctor recommended daily applications of testosterone to help mitigate that.
Hudson’s Guide has been around since 2004 and is the one resource I continue to go back to. Originally written with an FTM audience in mind as an homage to Lou Sullivan’s Information for the Female to Male Cross Dresser and Transsexual, they have since welcomed literally anyone else who might find the information useful. I highly recommend it for further research into the different ways testosterone can be administered and why people choose one way of administering it over the other, among other things.
What changes should I expect to see if I microdose testosterone?
When I invited people to send me questions for this piece online—some of whom gave me permission to use their own experiences with microdosing—some asked specific questions about changes they should expect. As I intend to keep reminding you, answering those questions is not so simple: Everyone’s body metabolizes testosterone differently, and, according to UCSFTC, genetics and age can also play a role in how effective hormones are. It’s also important to note that we all have varying hormone levels. It turned out that I naturally produce a higher rate of testosterone than the typical average for AFAB people my age, so testosterone likely worked a little “faster” for me.
The WPATH Standards of Care gives general timelines for specific changes, but acknowledges, “Most physical changes, whether feminizing or masculinizing, occur over the course of two years. The amount of physical change and the exact timeline of effects can be highly variable.”
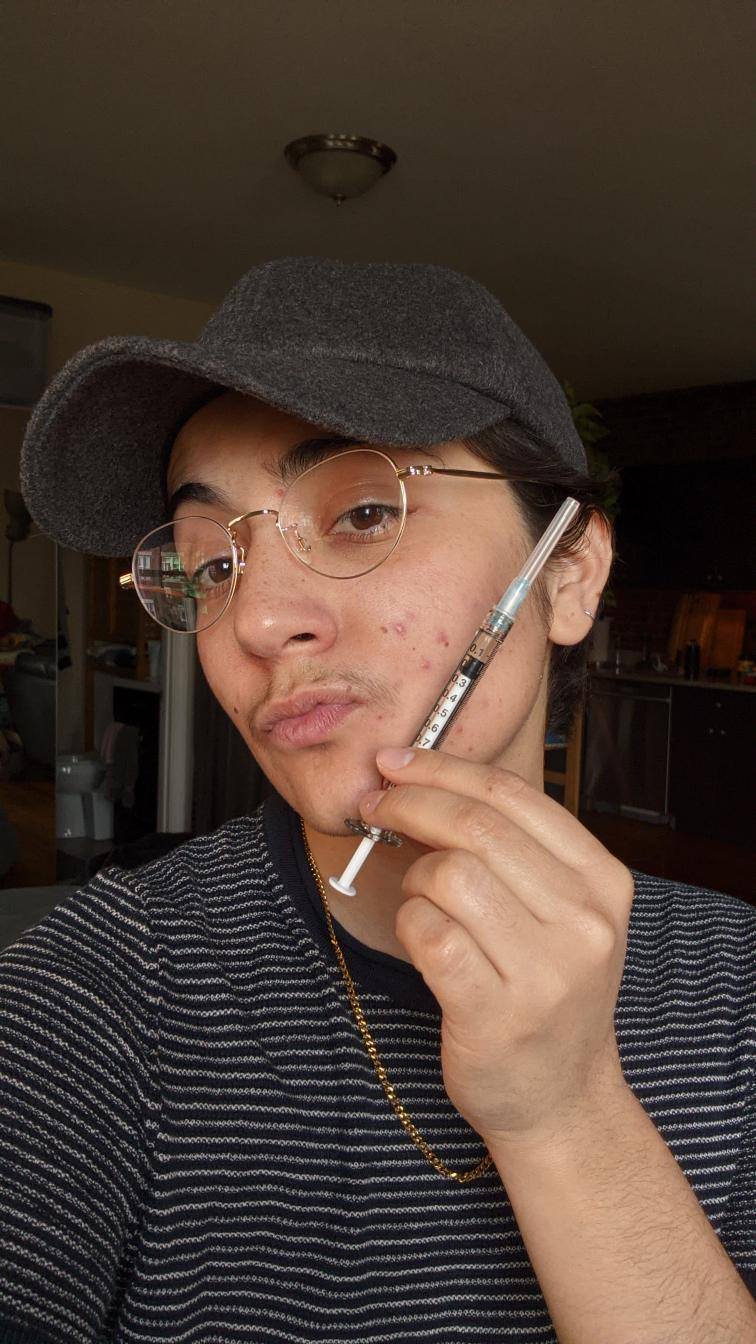
In microdosing for roughly three and a half years, I’ve experienced a wide range of changes—some quickly, and some more slowly—like more body and facial hair (most of which sprouted in the last six months), a very minimal voice drop, stronger legs, more stomach fat, a square jaw, more prominent cheekbones, a generally thicker physique, and acne (that has now subsided because I have a good skincare routine). Just to name a few.
Here are some very general guidelines for what physical changes you might experience when microdosing testosterone as an AFAB person. If you’ve ever done research about testosterone use in higher doses, you’ll definitely recognize the changes themselves—the point is that the process is a lot slower and more incremental, and that you probably won’t see more pronounced shifts, like growing a full beard.
Body and facial hair growth
Typically, when you’re taking T—whether microdosing or in larger doses— hair grows on your stomach, thighs, legs, arms, and face. If you want some frame of reference for how much hair you might grow, you can look around at other men in your family to get a good gauge, although this is harder to pin down when you’re microdosing.
Hair growth is inevitable. It will happen and… it’s irreversible! When I asked Colette Russen, the Medical Director of Community HealthCare Network’s East New York Health Hub, about the permanency of hair, she said, “I have a couple of… patients who have stopped T and… their facial hair does not go away.”
Senn Van Beek, a 31-year-old AFAB non-binary person from the Netherlands, told me their hair growth has been “kinda intense, but also not.” They have been microdosing for roughly three months and have grown thigh hair, stomach hair, and a few fuzzy facial hairs, but no thicker or longer arm hair.

By contrast, though I’ve been taking T for a longer time, I am only just experiencing an intense increase in facial and thigh hair, including a mustache that, to my disdain, reminds me of Justin Bieber’s. (Remember how everyone’s body metabolizes testosterone differently? There’s one example of how that works in practice.) Van Beek regularly sees their dermatologist for electrical epilation—a dermatological procedure that removes unwanted hair permanently—because they don’t like body or facial hair on themselves.
Vocal changes
Testosterone causes a thickening of the vocal cords, which can mean you develop a deeper voice. This is an irreversible change once it takes place, but taking any dose of T doesn’t necessarily guarantee that your voice will drop even one octave. For me, it’s been a hard change to track because I don’t often listen to my voice, but no one has ever pointed it out to me, so if there’s been a change, it’s safe to say it’s pretty subtle. If a deeper voice is on your goal list for your transition, UCSFTC has done a lot of research about vocal changes among trans people and runs two centers dedicated to vocal training and speech therapy—and hormones aren’t necessary for getting closer to where you want to be.
Bottom growth, sexual changes, and libido
(In this section, I am going to use scientific terms for genitalia.) I’ve found that not many AFAB non-binary people write or speak publicly about their experiences with bottom growth—which is a term for clitoral enlargement—during their transitions, but it’s an important change to acknowledge. (While you may think of erections as a function associated with cis men, clitorides can also become erect.) Bottom growth is typically between one to three inches across the board when a person is taking any dosage of T, and side effects can include more prominent erections. It’s an inevitable and irreversible part of the process of taking T. As I started microdosing, it was one of the first physical changes I noticed.
As Russen, the Medical Director of Community HealthCare Network’s East New York Health Hub, told me, “In the beginning, what you usually see or feel within three months to a year [is] that whole area gets really sensitive and painful… You can get erections at inappropriate times that are kind of uncomfortable.” (Russen also mentioned that patients should absolutely talk to their providers about what language they’d like to use when discussing genitalia.)
Personally, I don’t mind the growth, and the discomfort was short-lived, but I was a little self-conscious when sleeping with a new partner for the first time and found it useful to talk about it with them up front to avoid anyone being caught off guard.
Testosterone can increase your libido, but there are prevalent myths about testosterone, libido, and sexual preferences. You may have heard things like, “Testosterone makes you gay,” or, “Testosterone makes you really horny.” There’s actually no medical evidence to support any of that, and, in reality, human sexuality is extremely complex. During HRT, according to USCFTC, “You may find that different sex acts or different parts of your body bring you erotic pleasure. Your orgasms will feel different, with perhaps more peak intensity and a greater focus on your genitals rather than a whole body experience. Some people find that their sexual interests, attractions, or orientation may change when taking testosterone; it is best to explore these new feelings rather than keep them bottled up.” Your experience here will especially be your own.
The majority of the people I spoke to reported feeling more at ease in their bodies, which they said allowed them to explore things they previously would have felt too dysphoric to try.
Sex and sexual preferences are highly personal to begin with, so I would recommend documenting your changes as they happen by writing them down each day—or week, if you find it hard to maintain a daily practice. This is a helpful tool in understanding how your dosage might affect your sexual preferences, if it all. (We’ll come back to the subject of documenting later—it’s useful in tons of ways.)
Body shape and smell
Microdosing isn’t going to significantly affect the way your body is proportioned. If you’re top-heavy, chances are good that taking small amounts of testosterone isn’t going to drastically alter that.
When I first started microdosing, I expected to undergo drastic muscular changes despite not working out, and… well, nothing changed. In terms of muscle mass: You won’t turn into He-Man overnight, so to speak. Sadly, you’ll have to work for muscles if you want them, but muscle growth is a lot easier to achieve while taking T.
If a stronger body is something you’re after, it’d be good to also develop an exercise regimen. I haven’t yet figured this out for myself, but I like to find full-body workouts that don’t require any sort of equipment because I’m interested in generally getting leaner everywhere. If you are interested in finding workouts tailored specifically to AFAB trans folks, a quick Google search actually yields a ton of results.
Any additional muscle mass you experience from T itself is not an irreversible change and is highly dependent on how much testosterone you’re taking, your body, your diet, and genetics.
What you can expect to see in terms of your body fat: It redistributes, typically moving from the lower half of the body to the stomach area. If you experience dysphoria around your thighs or hips, T might help: Some people report their curves shrinking and a subtle, squaring of the body. Some report a flattening of breast tissue, as well, but going down whole cup sizes is pretty rare.
As far as appetite goes, the general anecdotal consensus is that appetite increases for a period of time because testosterone increases metabolism. Kei Rodriguez is a 28-year-old non-binary and genderqueer person. They’ve been microdosing T for six months and described feeling “voracious” for the first couple months. Their appetite has since leveled out, but they still eat more than they used to. For me, I didn’t notice a huge change—maybe because I’m a Taurus, so I already eat plenty.
Oh, and before I forget, your body odor may change. Mine did. It’s a little weird, but, in my opinion, it’s nothing to write home about.
Acne
If you’ve done some reading about T before, I’m sure you’ve seen a lot of information about acne and the effects that testosterone can have on it—aka, produce more of it. It was the one thing I was most afraid of when I first started, and, yes, my face did get oilier. I had pretty bad acne after six months of microdosing, but I was able to resolve it pretty quickly for two reasons. One: I went to the dermatologist for the first time and developed a more intensive skincare routine, which solved the problem in almost no time. The nice part about going to a dermatologist is that you don’t really have to disclose that you’re microdosing T if you don’t want to—you can just point out your acne, and they’ll typically know what to do. Two: “Generally, acne severity peaks during the first year of treatment, and then gradually improves,” according to the UCSFTC.
Mood
Mood is a tough one to nail down in terms of even general changes among people who microdose T, and, honestly, there aren’t a ton of studies or other research projects out there—something I’m hoping to see change in the next few years.
First things first, in terms of what we do know: There is a long-standing myth that testosterone makes you angry. This has been widely studied and hotly debated, but within the last few years, it seems that researchers aren’t so sure of the correlation. Accounts of ‘roid-raging bodybuilders are partially to blame for this correlation: It’s been verifiably documented that extremely high levels of testosterone can cause anger issues…… but, as I hope might be clear by now, that’s basically the opposite of what we’re talking about here.
Gray, a gay, agender, Black transmasculine 30-year-old, said they struggled with anxiety prior to microdosing testosterone. After beginning their transition, they said, “I still have anxiety. However, things just don’t get me to like they used to. When things do get to me, I feel like I’m more level-headed and able to process them better.”

If you don’t like therapy or have had bad experiences with it, that’s perfectly OK! Trans and non-binary people have long been overly pathologized in the mental health field, which is why I suggest finding a very knowledgeable provider who you can talk to about your mental health concerns in addition to your physical goals. In fact, let’s talk about that now.
How do you find a doctor and access hormones?
I asked Russen what advice she gives, as a medical director, to non-binary people who are seeking out hormone treatment for the first time. She said, “Do your research and find somebody who has some experience or works in an organization that has experience working with trans people, and then just really stick to your non-binary guns.”
Yeah, that.
Talking to a provider about microdosing was, in my experience, scary and overwhelming. If you feel unsure or afraid about how a doctor might react to this idea—or to you—that isn’t your fault. As we discussed, a lack of access to health care plagues the trans community; gender-affirming health care, outside of large cities with dedicated LGBTQ centers, can be difficult to find. Reading everything you can get your hands on about hormones and providers before you make an appointment can help you feel surer of yourself.
Finding a provider can be tricky, especially if you’re looking specifically for in-person visits, but here are a few good places to start:
Plume, a telehealth trans healthcare provider, is one of my top recommendations if you live in a more rural area or another place where LGBTQ people are particularly underserved in terms of healthcare. It’s also just a great telehealth option. I spoke with Plume’s co-founder and chief medical officer, Jerrica Kirkley, for this article, and I was pleasantly surprised by her dedication to providing GAHT for all patients, including people looking to microdose T. The one thing to note is that Plume doesn’t accept insurance and charges a flat fee of $100/month.
Centerlink provides an extensive list of LGBTQ healthcare clinics across the country, and clinics are usually a good place to start when searching for a primary care provider.
WPATH’s provider database goes beyond North America and, from what I can gather, seems to be regularly updated.
With any potential or ongoing medical provider, you should be fully transparent about your experiences and your identity so that they can help you figure out the best solution based on your physical goals, medical history, mental health concerns, and financial barriers. Based on your specific history and needs, the medical professionals you see should also thoroughly explain the process and all of the associated changes and risks.
WPATH’s Standards of Care states, “Ultimately, masculinizing hormone therapy is best undertaken in the context of a complete approach to health care that includes comprehensive primary care and a coordinated approach to psychosocial issues.” My argument for finding a dedicated primary care provider who has a lot of experience with gender-related care is that they’ll not only be able to help you with microdosing, but also provide holistic care with an understanding of your medical needs beyond hormones.
When asked about their experience with a PCP, Rodriguez said, “I’m lucky to have a trans-affirming primary care provider who practices informed consent, and I had a prescription for testosterone after a single telehealth appointment.” At my first appointment with my primary care doctor, they informed me that the amount of T I was taking would never result in getting rid of my period, and suggested another medication if that was a goal of mine, which was helpful to know.
If you feel comfortable with it, find a friend who can provide moral support as you navigate your feelings around different steps of the process and help you stand your ground if you run into any unwilling providers, whether they’re there with you in person or over the phone.
Jesse Lackowitz Crozier is 35, based in Brooklyn, and has long identified as non-binary… or something close to it. (It was actually in conversations with them that we first started using the word “microdosing” together!) They said having a friend support them as they sought microdosing treatment was key.

According to Crozier, the first time they sought out a low dose of testogel, it didn’t go well because their doctor insisted on prescribing an injectable dose more common for maximal effects. Crozier left the appointment feeling confused. “I was very freaked out. I called my friend when I got outside, and they were like, ‘Go back in there and be like, ‘You have to give me the gel.’ So I went back inside and [the doctor] was really pissed—[but] he gave me the gel.” Crozier promptly switched providers and are much happier now.
I’ve started microdosing T! Now what?
So you just did your debut shot or rubbed testogel on for the first time. Nice.
You should document your time on testosterone. This ethereal existence requires journaling! No (yes), but really, it’s important to write down the changes you’re noticing so that you’re able to keep track of what’s happening in your body and figure out if you’re on target with your goals. While there’s no exact formula for journaling, it’s helpful to track large-scale physical changes, your mood, and when you’re taking T. I keep a physically written journal along with a schedule of when I take T so I can keep track of how T might affect my moods. You can also take photos of yourself along the way, as opposed to hoping that you’ll notice tiny changes as they happen—with such a subtle process, being able to study still images can offer satisfaction that looking in a mirror can’t in terms of determining progress.
Documentation also serves as a helpful reminder of that progress when it feels like you’re “not seeing” the results you started microdosing to develop. Something I tell myself when a more impatient mindset takes over is that some changes are permanent, and I’d rather slowly grow body hair than blink and realize I’m covered in hair and I hate it. The point here is to ensure you understand what’s happening to your body so that you’re better able to judge—and inform your thoughtful provider about—how your dosage is affecting you.
What happens if I stop microdosing testosterone?
Of the people I spoke to for this piece, I’m the only one who has been on and off testosterone several times. In my experience, nothing stark or severe happens, but there are certain changes that came about from microdosing that go back to how they were before I started. Others don’t.
To quote UCSFTC, “Some of the effects of hormone therapy are reversible, if you stop taking them. The degree to which they can be reversed depends on how long you have been taking testosterone. Clitoral growth, facial hair growth, voice changes, and male-pattern baldness are not reversible.”
Some things that were affected when I paused T microdoses: My fat definitely redistributed again, I was less oily, and my skin cleared up (albeit, never back to how it was before I microdosed for the first time). I don’t typically experience any sort of raging dysphoria if I stop, as my face shape and hair growth are permanent.

It’s hard to find exact information about the length of time that someone has been taking T and how it affects them because of that pesky “hormones affect everyone differently” thing I keep mentioning. So you should really document everything. This offers you the ability to track what’s changed for you, specifically!
I like to think of microdosing testosterone as a form of body hacking, placing it in a lineage of trans ancestors who had to do the work of modifying their bodies themselves before there was any accessible care. For so many trans people, feeling at ease in our bodies has been difficult and sometimes impossible–historically, but also presently.
It has taken non-binary people a long time to have the option to microdose testosterone, which is, in itself, an exercise in patience: This was never about point A to point B. Instead, microdosing T allows non-binary people to access an in-between space that, for many of us, previously felt out of reach—but is right where we want to be.
Follow Alyza Enriquez on Twitter.
More
From VICE
-

Screenshot: Square Enix -

(Photo by AFP via Getty Images) -

All photographs by Adam Rouhana -

Getty Images


