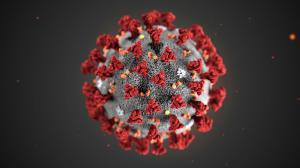
Ever since researchers have begun studying the virus and the pandemic, they’ve noted how the coronavirus is more fatal for men, particularly older men—they are at a much greater risk of dying from the virus than women who are just as old. Despite the observation, they had not been able to clearly pinpoint why.
But a new study that has been published on August 26 in the journal Nature has turned up a new clue. The research notes that globally, men account for about 60 percent of deaths from COVID-19 and explored whether differences in immune responses could explain why.
Videos by VICE
Men and women indeed develop different types of immune responses to COVID-19, according to the study’s lead author and immunology professor at Yale University, Akiko Iwasaki. Researchers collected nasal, saliva, and blood samples of 98 subjects—non-infected control subjects and patients with the disease who were treated at Yale New Haven Hospital in the United States. They then monitored patients to look at their immune responses.
The scientists found that women mounted a more robust immune response involving T cell (also called T lymphocyte)—a type of white blood cells that can recognise viruses and eliminate them. Women mount faster and stronger immune responses, perhaps because their bodies are rigged to fight pathogens that threaten unborn or newborn children.
Importantly, they found that poor T cell response negatively correlated with patients’ age and was associated with worse disease outcome in male patients, but not in female patients. “You could imagine scenarios where a single shot of a vaccine might be sufficient in young individuals or maybe young women, while older men might need to have three shots of vaccine,” said Dr Marcus Altfeld, a german immunologist.
Men also produced more cytokines, which are inflammatory proteins that form another part of the body’s natural immune defence. But “cytokine storm”—a situation where the immune system goes into overdrive and is harmful and potentially deadly—has been linked to severe cases of COVID-19. “Higher innate immune cytokines in female patients associated with worse disease progression, but not in male patients,” says the study.
According to the authors, this could imply that men and women need different treatments. For men, Iwasaki says in a video, “We should be enhancing their T cell responses with vaccines,” while women could be given treatment to dampen the cytokine response.
However, the study is not without its limitations. It only studied 98 participants; moreover, the average age of the subjects was higher—around 60.
Not all scientists agree to the result of this study, either. Eleanor Riley, a professor at the University of Edinburgh, told AFP that some of the divergence noted in the study is “likely due to differences in age or BMI (the sex differences disappear once these other factors are taken into account)”, and that others could have arisen “by chance”. This is why, she added, treatment shouldn’t be defined solely on sex and instead be individually tailored.
Other previous studies into why men seem to be hit harder by the coronavirus have pointed to female hormones such as estrogen and progesterone possibly providing women some protection against COVID-19, as also social and behavioural factors like the fact that far more men smoke than women or that men are more reluctant to see a doctor.
Follow Satviki on Instagram.