The UK government has been accused of hypocrisy after advising that under-30s be offered an alternative to the Oxford-AstraZeneca vaccine, due to concerns over extremely rare blood clots. Many have pointed out that the combined contraceptive pill comes with a greater – albeit still low – risk of clotting.
Yesterday, the Joint Vaccination Committee and the Medicines and Healthcare products Regulatory Agency (MHRA) announced that young people who are not at high risk of becoming seriously ill from COVID should have the option of a different jab. This followed 79 reports of rare blood clot cases out of 20 million people who had received the Oxford-AstraZeneca vaccine.
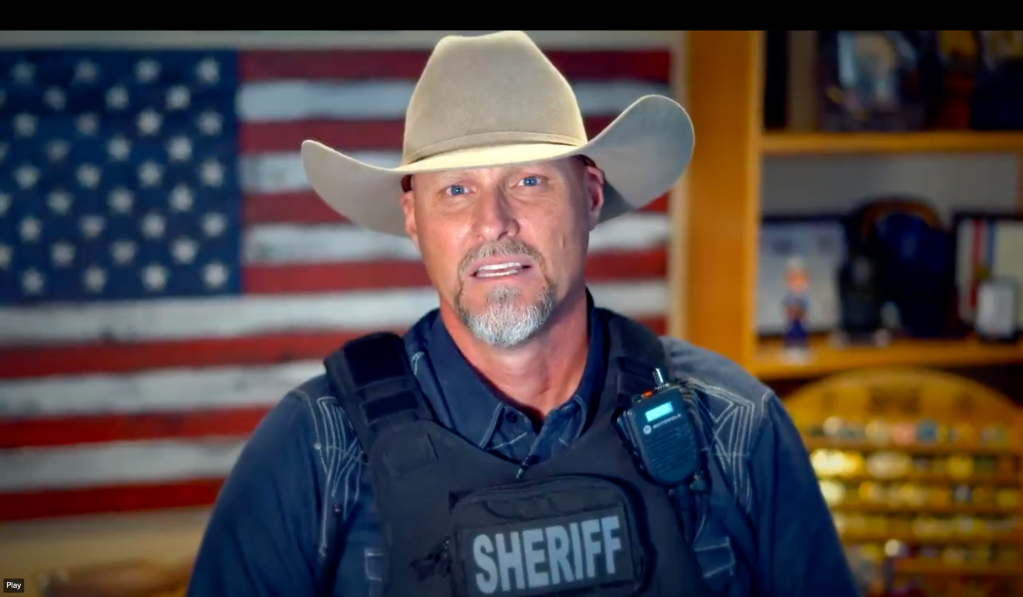
Videos by VICE
In comparison, the risk of blood clots in those who take the combined contraceptive pill – an oral contraceptive that uses estrogen and progestogen to restrict egg production – is around six in 10,000, according to a study in the British Medical Journal. One of the most widely prescribed contraceptives in the UK, more than 3.1 million women in England took the pill between 2017 and 2018.
VICE World News asked NHS England why the Oxford-AstraZeneca vaccine is regarded as a risk for under-30s, when people with uteruses continue to be prescribed the contraceptive pill. NHS England told us to speak to the Department of Health and Social Care. When we approached the Department of Health, they referred us to the MHRA. The MHRA then referred us back to NHS England for comment.
Many on Twitter accused government health officials of double standards in advising against the Oxford-AstraZeneca for young people, when contraceptive pills are prescribed with comparably far less caution. Journalist Jane Bradley wrote: “OK but why has the government been fine with letting all of us women take the contraceptive pill since our teens.” The tweet received over 49,000 likes and 7,000 retweets.
Reproductive health charities also took issue with the government’s unequal treatment of blood clot risks. Dr. Emma Chan, reproductive and sexual health lead at the School of Sexuality Education, said: “The difference in attitudes to potential risks and harms posed to the general population, as opposed to when we’re only talking about those with a womb, is really telling. It speaks to the problematic history of medical intervention and what its priorities and concerns are.”
“Although the reaction to vaccines is a really powerful example, it’s by no means an isolated case,” she added. “The situation around contraception in general is really problematic. Healthcare systems often focus on effectiveness, rather than patient acceptability and side effects of different methods, for example.”
Jonathan Lord, medical director at MSI Reproductive Choices UK (formerly Marie Stopes International), said: “In both the vaccination decision and in prescribing contraception, all the factors need to be weighed up for each individual, with alternatives considered alongside.”
“The combined oral contraceptive pill does have a higher thrombosis risk than other contraceptives, however this risk is significantly greater in pregnancy than in those taking the pill, and the benefits of the pill to many women is huge,” he continued. “For anyone with higher risk factors, there are alternative oral contraceptives which give no increased clotting risk and suit most very well. The essential element is that contraception and quality advice are readily available. Being able to access this – and having the really effective and convenient long-acting reversible methods available without a long wait – is where the priority should lie.”