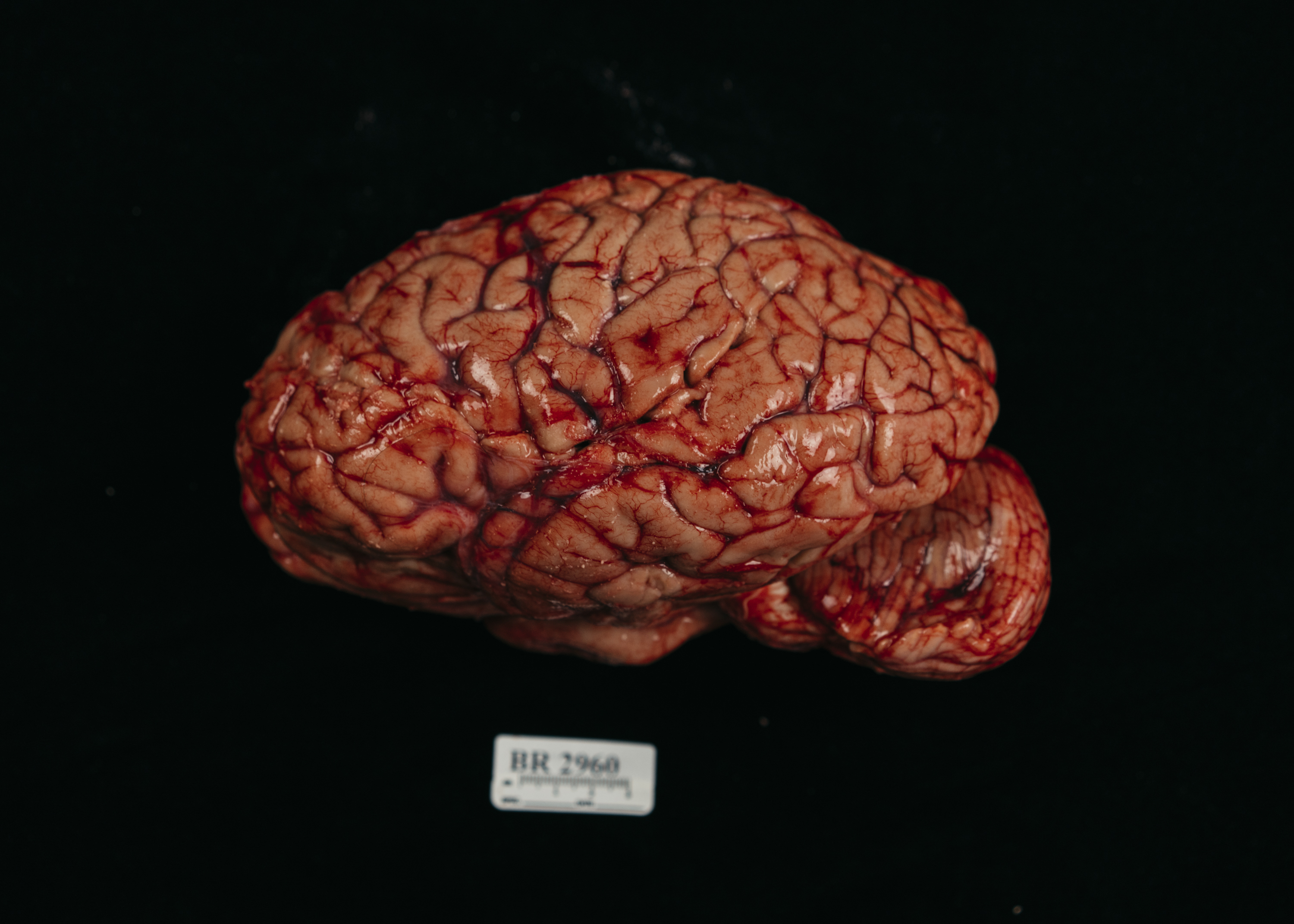
Less than a foot away from me, Jonathan Sirovatka pulls out a whole human brain from a red cooler packed with crushed ice.
I am at the NIMH’s Human Brain Collection Core (HBCC) in Bethesda, Maryland, watching as Sirovatka, who is the donation coordinator, processes a new brain donation. He scoots past me while I stand agape at the three-pound piece of flesh in his gloved hands.
Videos by VICE
I had not thought much about when, or if, I might ever see a human brain, even though I write about the brain’s function frequently. The brain can be regarded as an object of mystery, a black box locked inside our skulls that runs the show. It is, in many ways, our version of the soul. It’s where our personalities and consciousness are contained, and where abstract feelings like gratitude, familiarity, or fear take physical form in our brain regions and circuits.
And yet, seeing it here—alone, out of the skull, detached from the brain stem, it’s overwhelmingly fleshy. It’s a bulging mass that spills over the edge of Sirovatka’s hands as he cups the whole organ.

Of course I knew that the brain was made of flesh. But we so often refer to it as a “computer,” to its advanced “connectivity” and “plasticity”; I almost expected him to pull out a complex piece of machinery. Something less… meaty.
The day before, Sirovatka received a phone call from a Medicolegal Death Investigator at a medical examiner’s office in Virginia, who told him about a woman who had passed away. Sirovatka then called the family himself—in this case, her husband—and after getting his consent to donate his wife’s brain, he drove to pick up the brain in a government car. The brain rode back with him on the floor in the back seat of a Chevy Sedan. The HBCC can’t take brains that are more 48 hours old, so Sirovatka usually calls the family within 24 hours of a person’s death.
Sirovatka had returned to the NIMH with the brain at 11:30 that morning, and I arrived by train one hour later.
“This is what we would call a control individual,” Sirovatka tells me. He’s looking at the brain closely and picking off small stringy fibers from its exterior. “She had no medical history. She was not mentally ill. And she passed away suddenly; my guess is for cardiac reasons. And so that would be for us a very good individual by which to look at a normal brain function.”
The first time Sirovatka saw a brain, he was 16. He walked into a room just like the one I was currently in at NIMH, where a doctor was performing the same examination he was now doing.
“The first thing she said to me was, ‘Oh come and look at this brain, it’s a beautiful one, this is a great one.’ And I thought at the time, That’s a really weird thing to say,” he remembers. “But now, I have come to appreciate it at that level. When I see a particular brain, I can say, This is a really good specimen.”

What makes a “beautiful” brain? It should be well-preserved, meaning the body was kept cold. The flesh should be firm, not too soft. It shouldn’t be overly congested with blood, or swelling with water or other fluids that might build up. “I liken it to a carpenter working with wood,” he says. “You might have a piece of wood with all the grain going smoothly, and another piece with a knot in the middle of it.”
Sirovatka is now making sure there isn’t anything wrong that’s been missed with this brain. He examines the blood vessels, looking for yellow buildups of fat, or plaques, that might be present in a person with high blood pressure. He also scans the brain for any bleeding, bruises, contusions, anything that’s too big or too little. Women’s brains are a little bit lighter than men’s, 1200 to 1300 grams compared to 1300 to 1400, or a range of two to three pounds. He says that occasionally they might find something like a tumor or an aneurysm and help determine what an unknown cause of death was. Then he touches the brain lightly all over, feeling for if anything is too soft, or too hard.
The consistency, if a brain has been kept cold enough, should be firm, he tells me. “Kind of like gelatin that’s in the refrigerator, like Jello.”
The purpose of the HBCC is to study the underlying causes of mental illness, something its director, Barbara Lipska, knows all too much about. In January of 2015, her doctors told her that melanoma had metastasized into her brain. She had developed more than 20 brain tumors that altered her behavior and personality. She’s now in remission, but as we sit to talk outside the room where Sirovatka is inspecting the new brain, she tells me it’s reinforced for her how important the work they do is.
“When I lost my mind, I understand fully what it is not to have it,” Lipska says. “And I know that I am contained in my brain. Or even just parts of my brain, which were swollen and inflamed. It gave me this really materialistic lesson. If you lose yourself, that’s what it is.”
For mental illnesses like schizophrenia—which Lipska has spent her career studying—we don’t yet know what changes in the brain lead to the illness. While imaging techniques of the human brain have improved a lot, they don’t get at the brain’s molecular underpinnings: its DNA and RNA, the genetic sequence and its expression that could vary slightly in people with mental disorders.
That’s the bulk of what they do now, Lipska says. Collect, sample, analyze, and compare. But for any genetic study, you need a lot of samples. They’ve published numerous papers on subtle differences they’ve uncovered in the brains of the mentally ill compared to controls. But what does it mean? They’re just starting points on a very complicated path that will take more brains to lead the way.
“We have no doubts in our minds that mental illness problems are located in the brain,” Lipska says. “They’re physical changes in the brain. Unfortunately we don’t know yet exactly what they are.”
The HBCC has existed in some capacity for more than 30 years, and is one of a handful of brain banks across the country. But the need for brains is still high. Last year, the NIMH put out a memo “addressing the urgent need for brain donation.” People donate brains less than other organs, in part because the process can be difficult, because they’re worried about damaging their loved one’s appearances, or that they’re giving up an organ so closely related to our identities.
In 2013, several institutions collaborated to form the NeuroBioBank, to help organize, collect, and distribute brain tissue and make it easier on donor families to do so. “I understand why it is very different from agreeing to donate your eyes, or your kidneys,” Michelle Freund, the director of NeuroBioBank says. “It’s what I think makes me me.”
There are six partners that collect brain donations, and they can all be contacted for samples by researchers. The HBCC is separate than NeuroBioBank due to an odd bureaucratic fluke (it’s part of NIH’s intramural programming, while the NeuroBioBank is extramural). Freund says that means only they get their funding differently. If a researcher in the community wants tissue samples, they can ask either group to try and get what they need.

Each site of the NeuroBioBank collects about 100 brains per year. Sirovatka tells me that they get a brain at the HBCC, on average, every week or so; about 70 to 80 per year. But it’s not a guarantee, and they’re constantly aware that they’re working with a finite, non-renewable resource.
Even though Lipska stresses it will be a long road to uncovering mechanisms to our mental diseases, even with brain donation, valuable discoveries are already being made with brain tissues. In 2015, a lab at Harvard sequenced the genome of individual neurons from postmortem brains, and found that each neuron has many small changes made to it over time, called somatic mutations. This could act as “a durable and ongoing record of neuronal life history,” the paper said, and there’s now investigation as to whether these mutations contribute to any brain disorders.
Another recent finding was the discovery of a genetic risk factor for schizophrenia, called C4, which is one of the strongest signals for a risk factor ever found. “It has been virtually impossible to model the disorder in cells or animals,” said Steven McCarroll, the lead author on the paper, in an NIH press release.
Freund tells me that while a lot of NIH funding goes into mice studies—and they’re critical at the beginning stages of research—“there is no such thing as a schizophrenic mouse,” she says. We can study animals that model certain behaviors in schizophrenia or any other mental illness, like bipolar disorder or major depressive disorder. But at a certain point, we need to turn to the human brain for answers. The C4 findings used the genomes of 65,000 people and 700 postmortem brains to help power their genetic results.
Before we watch Sirovatka begin to cut into the brain, Lipska tells me, how “awesome” it is to be able to work with human brains, the very stuff in which all the secrets lie. “I am a materialist,” she says. “I’m not spiritual in the sense that I don’t believe that there is a higher power that makes us do things. I believe that everything is in this piece of flesh that you saw. But how it can happen? How does it dream, love, smell? It’s more, in my mind, a question to the future of generations of neuroscientists than to philosophers. But maybe both.”
Sirovatka places the brain onto a plastic contraption, called a cutting mold, that will allow him to make slices of exactly the same size: “parallel, consistent, and symmetrical,” he says. As he begins to pass the blade through the brain, I ask him what it’s like to call the families. This brain so recently belonged to a person, was a person, and that person belonged to other people. I’m finding it powerful that Sirovatka—who made the call—is the same person now dissecting the brain. It wasn’t something that was outsourced to a call center, or staffed with receptionists making dozens of calls a day.

Sirovatka pauses with the blade and tells me that making the calls is the hardest part of his job. “This is a call they’re not expecting,” he says. “Sometimes, I’m calling the family of a homicide victim, so it’s a tragic and dramatic death. Often times it’s not a well-received phone call. I mitigate that by showing the utmost respect; be sensitive, empathetic.”
A frequent cause of death that the collection is receiving right now is from accidental drug overdoses, from either opioids or mixtures of alcohol and Xanax. Those brains often come from people in their 20s. After overdoses, many of the brains come from people who died from suicide: About 34 percent of the brains they have are from suicides, 23 percent natural deaths, and 11 percent homicides.
But these phone calls can also connect him to the patient, perhaps more than even handling their brains.
“It’s rewarding and it helps me to remember that these are people not just lab specimens,” he says. “When I call them I start out by introducing myself, and where I’m calling from. I explain to them how I got their phone number and I express my condolences for their loss. It’s very important that when you do that, that it’s not a scripted line, but that I genuinely mean it. So before I call, I’ll just kind of pause, and I’ll look at the information and tell myself, ‘You’re calling a mother who has just lost her 20-year-old son.’ I center myself and recognize who I’m calling and what they might be feeling.”
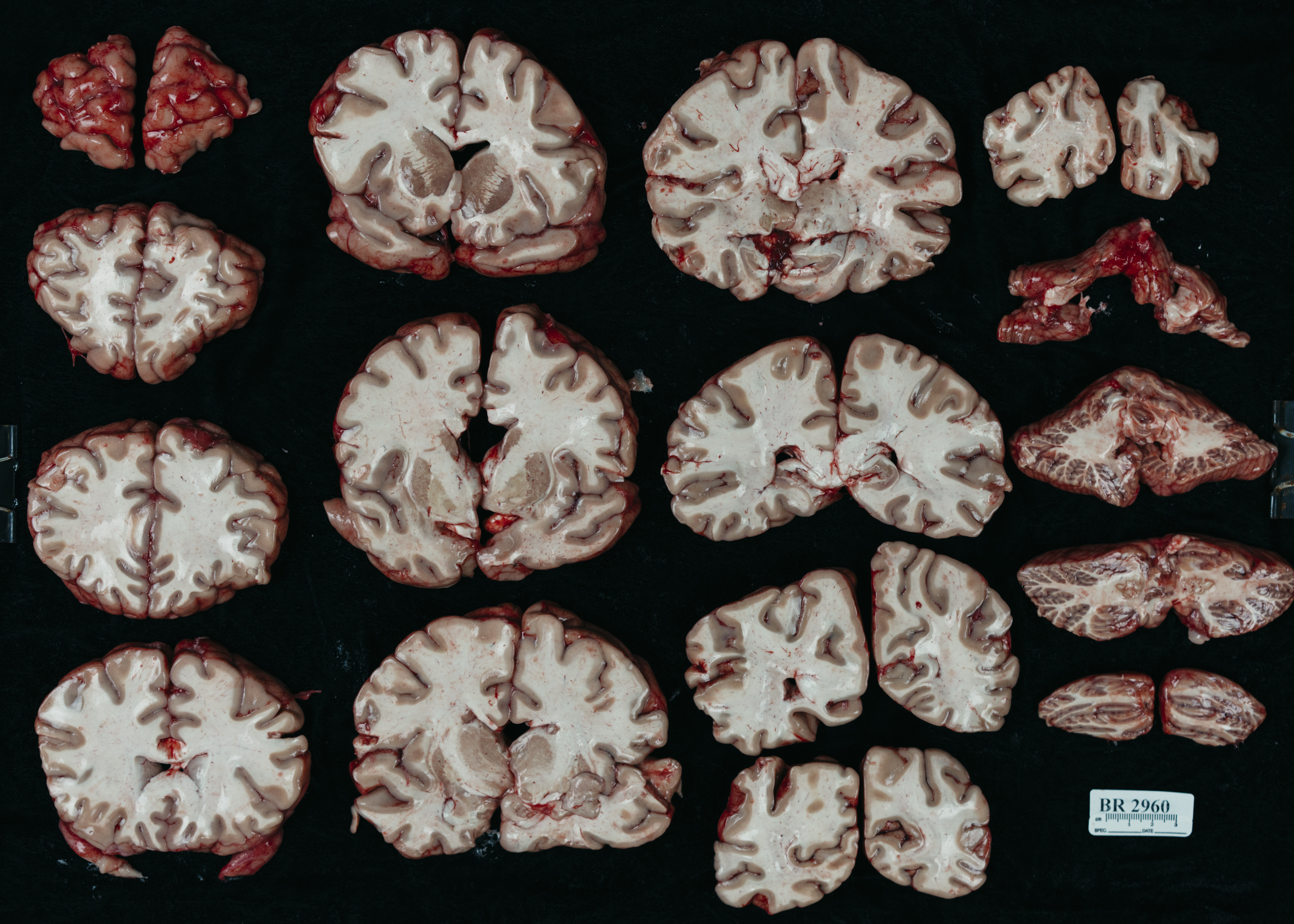
Sirovatka lays out the pieces of the brain and gently dabs blood off so all the inner structures can be seen easily. He’s arranging the slabs on a black cloth from the front—the forehead—to the back of the head. And tells me the most requested parts of the brain by researchers: the prefrontal cortex, the hippocampus, basal ganglia, and anterior cingulate cortex.
At this point, the brain is beginning to take on a more sterile look. It’s not bloody anymore, and it’s cut into pieces that resemble images I’ve seen in textbooks. The inner workings of the brain branch out, almost like pieces of coral. Rather than pink, fleshy, and alive, it’s now grey. Now, Sirovatka begins a process called flash-freezing.
First he separates the two halves of the hemispheres. Some pieces are set aside for microscopic evaluation, and go into formalin solution that stops them in time from degrading. The rest, Sirovatka places on a piece of glass to keep them flat and dips them into a solution of dry ice and methylbutane, which is minus 78 degrees Celsius. When the pieces drop in, the solution bubbles, and it looks like it’s boiling. But Sirovatka tells me it’s actually the opposite: It’s freezing so fast that I’m seeing any remaining heat transfer out of the tissue. The frozen chunks are placed into baggies, labeled and put away in storage.

All wrapped up in his apron, mask, and gloves, it’s hard to get on a read on Sirovatka and how he feels cutting into and dissecting an organ that we give almost magical qualities. You can tell he has done this so many times. He’s worked at the collection for 14 years, and he moves with ease handling the brain pieces.
Sirovatka tells me that on a certain level, he is desensitized to working with brains. Like any job, if you do it long enough, it gains some kind of automaticity. But if he stops to think—with the very organ he is currently dissecting—the wonder isn’t lost on him.

“I heard someone say once that the brain is the only organ that’s aware of its own existence,” he says. “I had never really thought of it that way and it was fascinating. Your heart doesn’t know it’s a heart, or that it exists. So when I first take it out of the transport container, and I’m holding this entire brain, I do pause, and it’s kind of like a wow moment. This is what I’m holding. It’s incredible. It really is incredible.”
Sign up for our newsletter to get the best of Tonic delivered to your inbox.
More
From VICE
-

Ru Callender leads a procession through the streets of Liverpool for the KLF's annual Toxteth Day of the Dead celebration. Photo by Thomas Ecke -

Ranchers in Colorado (Photo by Helen H. Richardson/MediaNews Group/The Denver Post via Getty Images) -

Lauren Levis, who died after taking iboga at the Soul Centro retreat in 2024. (Photo courtesy of the Levis family) -

Collage by VICE
